Saturday, August 11, 2007
Bye bye and Thanks
First, I would like to thank Drs. Wang and Frayer for instituting such a program – I absolutely loved my experience this summer. There was so much I learned about medicine, surgery, health care, how engineers fit into health care, human dynamics, myself, etc., etc… not to mention, being able to enjoy New York City in the summertime. If you haven’t noticed…this summer was priceless for me and I am very grateful to have had this opportunity. I also would like to thank Dr. Grant for being my mentor. Although, I enjoyed surgery in general, I found a special enjoyment out of plastic surgery and I think that can be attributed to having a great mentor and plastics squad.
I hope everyone else had as great of a time as I did this summer and best of luck to all of the future participants in the program. Get involved and enjoy the experience, you will probably never do anything like it again. That’s it all...for now...
Tuesday, August 7, 2007
Final Week of Summer Immersion...Tear
Anyway, as I showed in my presentation my research project basically consisted of a literature review and case study analysis to form the foundation for a prospective investigation of Dr. Grant’s. He wants to assess the effect short pulsed electromagnetic fields have on post-op breast augmentation patients. I won’t go into everything that I presented on; however, some of the more interesting findings were as follows. First, was a meta-analysis of over 30 years and 50 clinical trials on both bone and soft tissue revealing that ALL studies were methodologically flawed…awesome. I’m glad published research is so well reviewed…and carried out for that matter. Some of the flaws were huge, too – like no control groups or errors in the protocols. Honestly, I thought that was outrageous. Nonetheless, these were studies from years ago, and a lot of the newer studies are much better designed. Several of the better, more recent articles showed that in vitro and in vivo PEMF stimulated the synthesis and upregulation of various growth factors, such as, platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), and transforming growth factor (TGF). These growth factors then act to induce cellular proliferation, angiogenesis, stimulation of an immune response, deposition of ECM and wound contraction. In other words, they aid in wound healing and in turn should also help reduce pain in human subjects by speeding up the healing process. The chart below illustrates an increase in tensile strength of rat wounds treated with PEMF for 21 days post-op as compared to the negative controls. Signal I, II, III, and IV are simply varying doses of PEMF; whereas the "Sham" is the negative control.
A company called Ivivi Technologies in
The electric field induces a magnetic field and the device is laid on the wounded area, applying the desired PEMF therapy directly onto the patient’s wounds. It’s a non-invasive therapy that allegedly reduces pain and speeds along the healing process, allowing for an earlier discharge, and thus, cutting costs, too…that is if it actually works. A cool idea. But, it just looks so bogus to me. Anyway, the company has just released news that they have an IRB-approved, randomized, double-blind, placebo-controlled clinical trial on 30 ischemic cardiomyopathy patients (decreased blood flow to the heart) who are not candidates for surgical procedures. If it works in these cases, that would be absolutely great…it could reduce the number of many invasive, difficult cardiac surgeries. Personally, I think the biggest obstacle with this technology will be convincing the general population that a stupid wire with a flashy LED on it will actually save you…
Sunday, August 5, 2007
Some thoughts about surgical staplers
Surgical staplers and clip appliers are complex mechanical medical devices that have been on the market for years and are mature in their technology. These devices are used in gastrointestinal, gynecologic, thoracic, and many other surgeries to remove part of an organ, to cut through organs and tissues and to create connections between structures. The benefit of using these devices allows for more complex procedures and shorter surgical procedure time.
However, Each year over the past 5 years there have been 8,000 to 9,000 adverse event reports related to surgical staplers. The most common problems with the device are: staples don't form, staplers misfire or don't fire. The most common problem with the patient is anastomosis failure. This is also where my research project originally arise from. Solving the anastomosis problem is meaningful.
In the OR, I also saw electronic surgical staplers. Compared to mechanical stapler, it provides improvements such as, removes force from the anastomotic site; digitally senses tissue compression levels; digitally selects staple heights; prompts surgeon via LCD and voice message.
By talking to the doctors and the engineers from the vendors, I feel that the research in a medical device company is somewhat different from research in the school. In the school, the research is more focused on the basic science, but in a company, it must be application oriented. For example, the physical principles inside a stapler have been well established since Newton and Maxwell. However, such a device is still innovative because it facilitates doctor’s procedures, and it fundamentally changed suturing process. The research is a designing process. Instead of incorporating a lot of high technologies, a device that best meets the doctor’s need might be more useful.
Friday, August 3, 2007
Neurological Surgery
Neurological Surgery
I also have been working on my clinical research project evaluating effectiveness of two different treatments for aneurysms, and have obtained some interesting results. I will be presenting my research project in the seminar meeting in
Overall, I gained a lot from this experience, especially in terms of realizing that there are many areas that still need technological improvements. I would like to thank my clinician mentor, Dr. Riina, and also Dr. Gobin and Dr. Chapple.
Thursday, August 2, 2007
Vascular Wrap-up
Week 7
The Last Post
Last time I left a taunting message about my research—now it’s time for some results! It turned out that the average age of the last menses was 48 and that surgery would occur within 20-29 years after this age with 99% statistical confidence. This identified the patient population with ages 68-77. The HRT data revealed that there was no significant difference between patients on HRT vs. not for primary patency while patients with osteoporosis were worse-off than those without osteoporosis. This is interesting data that may suggest that patients with osteoporosis who undergo vascular procedures should have more frequent patency check-ups.
This is the last post for me! One thing that I pulled away from this experience is that I do not want to be a doctor, at least not a surgeon! They have an intense lifestyle to say the least, and they basically live at the hospital. Otherwise I had a chance to see some great technology and procedures that I wouldn’t be exposed to anywhere else, and living on the Upper East Side rent-free was unbeatable. Thanks to Dr. Vouyouka, and thanks for reading!
Surgery and Adios
The summer immersion program is almost over now, and I think that I did gain a better understanding of clinical practice. I am fairly sure this experience will spill over into my current collaborations, and will benefit me. It also gave me a better understanding of the need to be assertive. The programs structure does need refinement, however, but it is not a loss, especially if one tries to gain specific insight on one’s own. It would have been nice if the exact clinical experiences we were expected to have (and it did feel as if there explicit expectations) would have been spelled out clearly before hand.
I’m looking forward to returning home to my wife and child tomorrow. Happy 1st birthday, Aiden!
Mitral Valve Replacement (MVR)
Finally, I convinced myself to watch at least one open heart surgery. I was surprised at how invasive the whole procedure was. The doctors’ basically sedated the patient, sliced his chest open, and then pulled his ribs apart using their bare hands or a crude mechanical device. It was almost like watching a scene out of a movie with hygienic zombies in scrubs trying to carefully eat the victim’s heart. Okay, maybe that’s an exaggeration. What followed was a bit more impressive. They bypassed the patient’s arteries, immobilized the heart using high concentration of potassium chloride, and then made an incision in the heart in order to replace the mitral valve. The following picture is borrowed from its.med.yale.edu. It depicts a mitral valve replacement.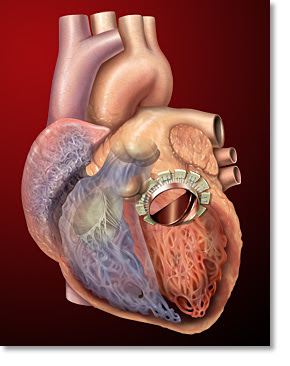 Apparently, this particular patient had mitral valve regurgitation. This was evident from his transesophogeal echocardiogram or the ultrasound measurements. One could see that the oxygenated blood that entered the left ventricle through the mitral valve periodically reentered the left atrium. In most cases, a patient’s valve is irreversibly compromised due to either ischemia, stenosis, or infection. These problems are usually onset due to coronary artery disease, age, or rheumatic fever, respectively. However, congenital defects are not rare.
Apparently, this particular patient had mitral valve regurgitation. This was evident from his transesophogeal echocardiogram or the ultrasound measurements. One could see that the oxygenated blood that entered the left ventricle through the mitral valve periodically reentered the left atrium. In most cases, a patient’s valve is irreversibly compromised due to either ischemia, stenosis, or infection. These problems are usually onset due to coronary artery disease, age, or rheumatic fever, respectively. However, congenital defects are not rare.
In the patient’s case, the problem was caused by ischemia through coronary artery disease. As a result, the doctor had decided to replace his valve with a bovine valve - the reasons for choosing a bovine valve or a mechanical valve were explained previously by Dickinson. It seemed as though the stitching of the valve required great dexterity. One of the more skilled residents tried to stitch the valve but it seemed as though he could not make the more difficult 10-12 o’clock stitches. As a result, the primary surgeon took over and showed him how it should be done.
One could definitely make it easier for these doctors by developing an innovative device for sewing. In fact, I don’t really know why a big hospital like NYP still uses open heart surgery for such cases. There are hospitals that are performing these types of procedures percutaneously using the da Vinci surgical system. I think that’s the way to go. If not, the least one should do is make something that replaces the “needle and string.”


